1. Choose the right metrics to compare performance
Remember also that gag clauses telling manufacturers or other actors to keep rebates secret are now forbidden. From January 2022 on, every employer can ask their PBM to disclose the rebates they negotiated and regain control over their passing through to themselves.
The takeaway is that rebates are not the right metric: you can get huge rebates and still pay more than others when the price list is higher, as shown in the example below:
Drug XYZ List Price : $ 1 000 at PBM A
Rebate 50%
Billed price = $ 500
——-
Drug XYZ List price : $ 750 at PBM B
Rebate 35%
Billed price = $ 487.5
——-
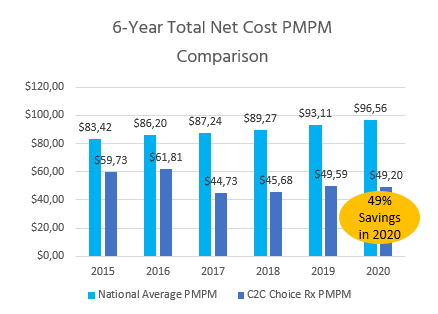
The right metric is: Total pharmacy cost Per Member Per Month (PMPM). Ask your candidate PBM to commit to the lowest possible PMPM objective.
Request a thorough past claims analysis and ask your partner to commit to cost targets, based on a comprehensive analysis of the formulary drug prices.
2. Ask for independent clinical advice to build and maintain the formulary
Our partner for instance has a Joint collaborative with an academic health system.
This protects the integrity of the plan from any conflict of interest due to the owning by the PBM of its Specialty pharmacy network.
3. Request regular Rx Plan recommendations
4. Use generics to your advantage
Make sure they use to their full extent the possibilities of the huge and highly competitive generic drugs market. For example, we average 98.7% generic fill success of target generic formularies. Don’t forget that PBMs don’t get any rebates on generics and will not always be eager to promote them.
This explains much of why a small actor, with lower buying power can beat the top 3.
5. Clarify your cost control strategies
They will include reference-based pricing and wasteful drug exclusions.
Your primary targets are the top 20 high-cost brand drugs.
6. Put pressure on specialty drugs prices
- Utilization Management through “real” step therapies and prior authorizations
- Copay optimization with manufacturer using copay or coupon cards
- Obtain funding from foundations for eligible patients with certain high-cost chronic conditions
- Help low-income patients to apply for Manufacturer Assistance Programs (MAP)
- Leverage huge savings via International pharmacy mail-order at licensed pharmacies
- Find qualified providers for infusions outside of hospital settings which often practice egregious markups on the medicines, on average 200%-300% over the Medicare reference prices.*
7. Negotiate a short, clear, unambiguous agreement banning all “bad” practices
Such as spread pricing, claw-backs, gag clauses, multiple administrative fees.
8. Ask for extended audit rights
Transparency is granted through extensive audit rights, as foreseen in the agreement. Request the implementation of a systematic control of the PBM adjudication system to prevent errors and fraud. The FBI estimated the amount of adjudication frauds to 10% of the entire health care spending.*
Check your contract and make sure it provides for adequate auditing processes.
Conclusion
Solutions still exist on the market, thanks to a new generation of PBMs who will act in the exclusive interests of the plan sponsor and its plan members. What is at stake is cutting your pharmacy budget in half, as shown below with our solution..