
Finally! Humira’s biosimilars also hit the us market!
Humira was first marketed in 2002 and was protected in the US market until 2023, thanks to AbbVie’s use of two strategies :

Remember also that gag clauses telling manufacturers or other actors to keep rebates secret are now forbidden. From January 2022 on, every employer can ask their PBM to disclose the rebates they negotiated and regain control over their passing through to themselves.
The takeaway is that rebates are not the right metric: you can get huge rebates and still pay more than others when the price list is higher, as shown in the example below:
Drug XYZ List Price : $ 1 000 at PBM A
Rebate 50%
Billed price = $ 500
——-
Drug XYZ List price : $ 750 at PBM B
Rebate 35%
Billed price = $ 487.5
——-
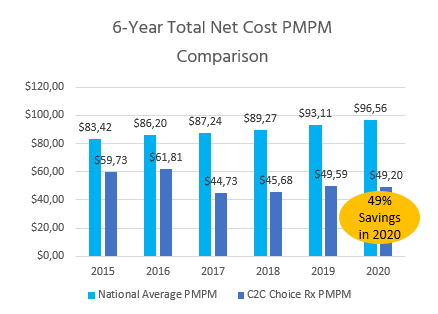
The right metric is: Total pharmacy cost Per Member Per Month (PMPM). Ask your candidate PBM to commit to the lowest possible PMPM objective.
Request a thorough past claims analysis and ask your partner to commit to cost targets, based on a comprehensive analysis of the formulary drug prices.
Our partner for instance has a Joint collaborative with an academic health system.
This protects the integrity of the plan from any conflict of interest due to the owning by the PBM of its Specialty pharmacy network.
Make sure they use to their full extent the possibilities of the huge and highly competitive generic drugs market. For example, we average 98.7% generic fill success of target generic formularies. Don’t forget that PBMs don’t get any rebates on generics and will not always be eager to promote them.
This explains much of why a small actor, with lower buying power can beat the top 3.
They will include reference-based pricing and wasteful drug exclusions.
Your primary targets are the top 20 high-cost brand drugs.
Such as spread pricing, claw-backs, gag clauses, multiple administrative fees.
Transparency is granted through extensive audit rights, as foreseen in the agreement. Request the implementation of a systematic control of the PBM adjudication system to prevent errors and fraud. The FBI estimated the amount of adjudication frauds to 10% of the entire health care spending.*
Check your contract and make sure it provides for adequate auditing processes.
Solutions still exist on the market, thanks to a new generation of PBMs who will act in the exclusive interests of the plan sponsor and its plan members. What is at stake is cutting your pharmacy budget in half, as shown below with our solution..

Humira was first marketed in 2002 and was protected in the US market until 2023, thanks to AbbVie’s use of two strategies :

After wrapping up the 2023 enrollment, employers are now planning their next moves to mitigate the continuously growing healthcare costs impacting their plans. This is particularly true for pharmacy costs.

PhRMA, a Big Pharma lobbying group, released an advertising touting that drug prices were not fueling inflation. To prove it, they produce the graphic below.
Care2Care secured a strategic partnership with an innovative, transparent, 100% pass-through PBM.
Adding to our expertise in international drug sourcing, we expand our offer to the full pharmacy benefit management.
